People allergic to insect venom need precision medical diagnosis and treatment
A team of researchers has elucidated individual profiles of allergy reactivity in patients that are not protected after treatment with immunotherapy. The aim is to improve medical treatment of people who are allergic to insect stings.

Approximately 30 per cent of the European population suffers from allergies and 3–5 per cent are allergic to insect venom. In Denmark alone, 50,000 people are at risk of severe allergic reactions if they are stung. The majority of people, however, are not aware of their allergy.
If aware of the allergy, they can currently be protected with an acute injection of drugs or a long-term treatment with an allergen vaccine. This treatment is relatively successful, but there are a certain number of patients that do not respond properly to treatment. The putative reasons remained unclear.
Insect allergy sufferers do not react to the same allergens and, in some cases, the treatment therefore has a reduced effect or does not work at all. A limited protection at worst can be fatal.
“Vaccines for immunotherapy today are often based on the natural sources such as venom from insects and can therefore contain very different amounts of allergens and even venom from different species of insects. All venom allergic patients are treated the same way by using insect venom preparations, and this sometimes is not ideal,” says Associate Professor Edzard Spillner.
Molecular knowledge for better drugs
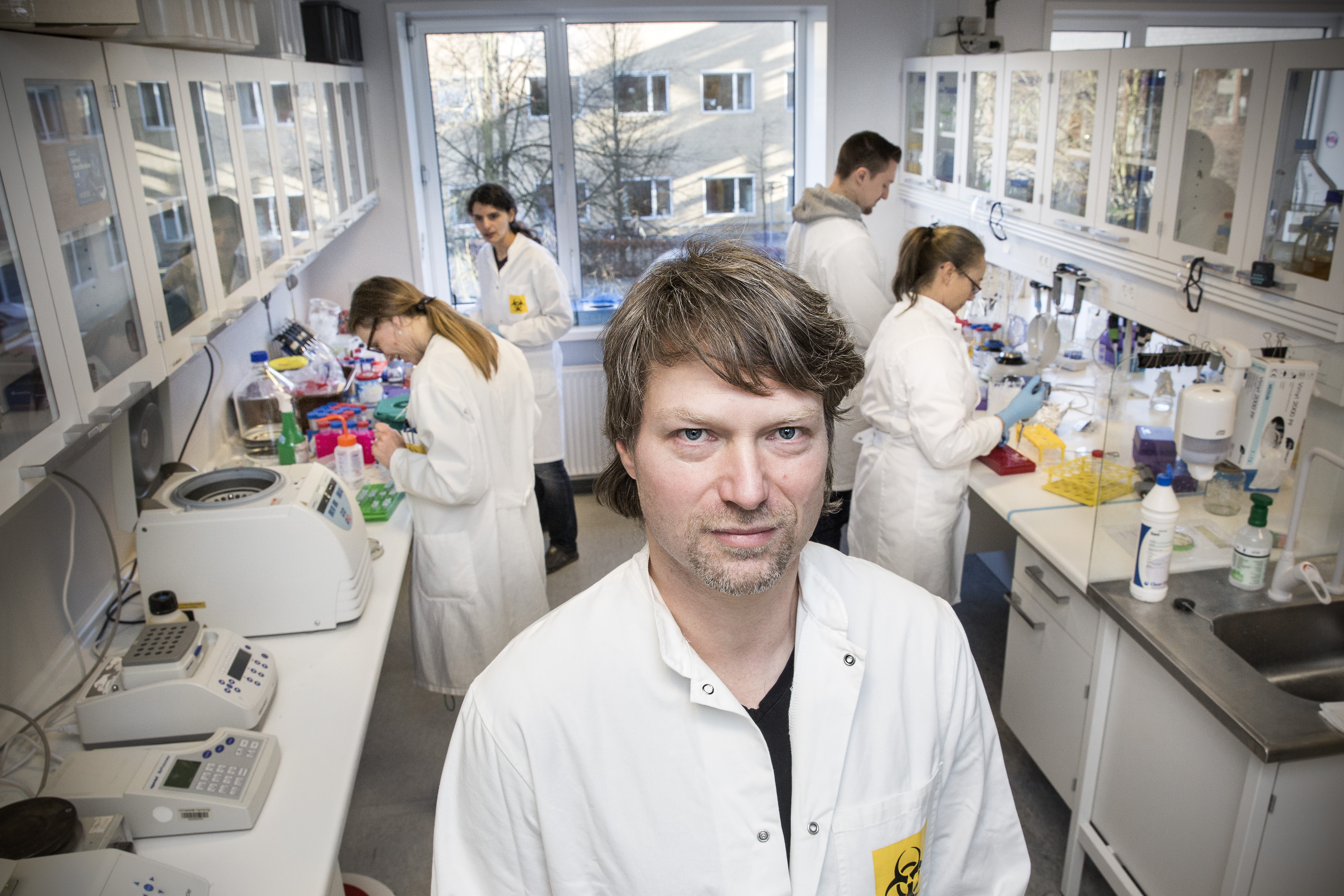
The researchers are therefore working on developing artificial allergens that perfectly mimic the allergens in insect venom. Associate Professor Spillner is an expert in the development and design of proteins for diagnostic and therapeutic use. In his laboratory at Aarhus University, he has produced a variety of artificial proteins for diagnostic and therapeutic purposes.
The research group also focuses on artificial human antibodies to insect venom allergens and other structures with relevance for allergic reactions. Here the known allergenic antibody IgE is particularly in the spotlight. In collaboration with other researchers at Aarhus University, the most interesting ones have been crystallized recently.
“We can isolate and rebuild IgE from the patient’s blood and identify the target structure it reacts with. This way we can analyse how it behaves together with the allergens. The better we understand the molecular mechanisms of action, the greater our chances are of developing new concepts in allergy treatment,” says Associate Professor Spillner.
The next step for the researchers is to describe precisely how the artificial antibodies bind to the individual antigens, and this can be the key to finding out by which factors the allergic reaction is driven.
Breakthrough in the laboratory
Using a set of several insect venom allergens, his research group and collaborators were able to carry out comprehensive mappings of the antibodies in patient sera that can cause anaphylaxis, and this is an important step in the direction of more and deeper knowledge of allergy, particularly to insect venom.
“After we can identify specific components of the venom as allergens and produce them artificially in the lab, we have routine access to studying the molecular processes going on in the blood of allergy sufferers. The component resolved approach is a major breakthrough in allergy and, in particular, in insect venom allergy and could be a benchmark for individualized immunotherapeutic treatment,” says Associate Professor Spillner.
The technology has the potential for improved and more extensive diagnostic practice. The researchers estimate that a large portion of people who are allergic to insect venom are currently unaware of their condition, and are unprepared for any severe allergic reactions that can occur when they are stung. Of those being aware and obtaining immunotherapy, those patients with specific recognition profiles could be identified which are at higher risk for unsuccessful immunotherapy using insect venom preparations.
Large study of anaphylaxis
In a large study involving several centres in Germany, Switzerland and Denmark, the researchers could show that in particular one of these components can be absent or significantly underrepresented in therapeutic preparations. Pronounced reactivity of the patient to one of the allergens, called Api m 10, has now been identified as a risk factor for therapeutic failure in honey bee venom immunotherapy.
This is good news for all allergy sufferers because the approach points to unsolved problems with therapeutic preparations. Improved preparations will probably be able to provide better protection of individual patients.
“We carried out our study in the field of insect venom allergy, but similar phenomena in principle apply for all kinds of allergies. We expect to extrapolate our results and use similar methods to study the scenario behind other allergic reactions,” says Associate Professor Spillner.
The results of the research have now been published in the scientific Journal of Allergy and Clinical Immunology.
Read the article in the Journal of Allergy and Clinical Immunology
For more information, please contact
Associate Professor Edzard Spillner, Department of Engineering, Aarhus University
